Abstract
background
Cryotherapy is a pain relief option commonly used in over-the-counter treatments for musculoskeletal pain management.
objectives
This study evaluated objective thermal skin response and subjective perception of cooling sensation with an OTC topical cryotherapy pain relief gel.
methods
A UK study of 50 healthy adults (aged 18–65 years) was undertaken with subjects acclimatised to a consistent baseline temperature before applying 0.5g of a commercially available pain relief gel (Biofreeze®) to their dominant forearm (test area). A baseline skin temperature gun reading was taken at the test area and over the next 11 minutes (every 30 seconds for 2 minutes, then each minute for a further 9 minutes). Thermal imaging of test and control areas was conducted throughout. After wash-out, subjects applied 1g of test gel to their opposite forearm, recorded time to perceived cooling sensation and completed a post-use questionnaire.
results
The topical pain relief gel reduced skin surface temperature from baseline temperature, with reduction detected at 30 seconds and at each time point interval, reaching a peak average 10.27% (-3.172°C) temperature drop at 4 minutes (p=0.05). The average time for subjects to record a cooling sensation after product application was 14.84 seconds, with 88% reporting cooling sensation within 30 seconds and 96% within 1 minute.
Conclusion
An OTC topical pain relief gel rapidly reduced skin temperature via objective thermal measurements and subjective perception. As skin temperature reduction can modulate pain pathways, this highlights the potential benefit of an OTC topical cryotherapy pain relief gel in analgesia management.
Full text
introduction
More than 150 conditions fall under the umbrella term musculoskeletal conditions (MSCs), disorders that affect the bones, joints, ligaments, muscles, tendons and spine1. According to the World Health Organization, such conditions affect an estimated 1.71 billion people worldwide and are the leading cause of global disability2. Among the most common MSCs are low back pain, neck pain, osteoarthritis (OA), gout, osteoporosis and rheumatoid arthritis (RA)2-5. The burden of MSCs on society is significant. In Europe, MSCs are the primary cause of years lived with disability and account for 38% of all reported fatal and non-fatal serious workplace accidents, with the majority of these due to sprains and strains5.
A particular challenge is the fact that the incidence of MSC conditions, such as OA, RA and low back pain, are directly linked to ageing3-6. As the global population is ageing, so the number of people living with MSCs is expected to rise3,4. For example, the Global Burden of Disease Study predicts a 74.9% increase in the number of cases of knee OA and an 80% increase in the number of people living with RA between 2020 and 20503,4.
Already MSCs exert a significant burden on healthcare. In Europe, a third of general practice consultations are due to a MSC and they account for 9% of all cases presented in hospitals5. This does not capture the wider burden of MSCs in the community, however, as data are lacking on the prevalence and incidence in community pharmacies, despite pharmacists’ role as the most accessible and frequently visited healthcare professional7. The advice and guidance of community pharmacists in helping patients optimise the safe and effective use of prescription medication is supplemented by their role as advocates of the use of self-care in pain management7. Self-care encompasses the use of non-prescription, over-the-counter (OTC) pharmacological pain management options, such as oral and topical analgesics, alongside lifestyle advice and non-pharmacological approaches7. The latter are a mainstay in MSC management guidelines for OA, low back pain, sprains and RA and include exercise, manual manipulation, mobility aids and the use of cold (cryotherapy)8-14. The predicted rise in the ageing population experiencing MSCs is also a factor to consider in pain management as older adults consume the most drugs and are at increased risk of medication-related adverse events3,4,15, therefore self-care options may play a greater role in the MSC treatment armamentarium.
Cryotherapy, or the therapeutic processes involving cold temperatures16, has long been claimed to have health benefits, dating back to Hippocrates17. In particular, cryotherapy, delivered via ice, cooling sprays or topical analgesics, has been used in the treatment and recovery from musculoskeletal injury and is recommended in guidelines for the relief of pain in sprains and strains as one of the key pillars within the RICE protocol (Rest, Ice, Compression, Elevation)18-21.
The local effects of cryotherapy include reductions in skin temperature, sensation, arteriolar vasoconstriction and tissue metabolism18. However, how cryotherapy reduces pain perception has yet to be fully elucidated but it is believed that cooling activates the body’s natural pain relieving pathways18,22-26.
What is known is that cold is detected in the skin’s somatosensory fibres by the Transient Receptor Potential Melastatin Family, TRPM827. This is a Ca2+ permeable, non-selective cation channel expressed in the dorsal root and trigeminal ganglia27-29. Modulation of TRPM8 activity has been suggested to be of relevance to the body’s analgesic response to cryotherapy29. The body’s cold-sensitive neurons are also sensitive to cooling agents, with animal data showing stimulation of the TRPM8 nerves by cooling agents activates the nociceptive pathway to promote analgesia28,30. Other research suggests cooling agents may also interact with other TRP receptors to contribute to an analgesic response31.
Given that the perception of skin cooling occurs with a 1°C reduction in normal body temperature30,32, this study sought to evaluate the objective and subjective cooling efficacy of an OTC topical cryotherapy pain relief gel in healthy adult subjects.
materials and Method
A monadic, central location test study of 50 healthy adults was conducted at the Sense:lab, Leeds, UK, on July 30th – August 1st, 2024. Subjects were recruited by an independent third-party product research agency, Blue Yonder Research, following an online survey of an established and verified consumer panel. Inclusion criteria were healthy, symptom-free adults aged 18–65 years (50% male; 50% female), non-rejectors of gel in tube format, non-rejectors of the test brand, previous users of menthol-containing products without adverse events (e.g. topical pain relievers, toothpastes, cosmetics and personal care products) and able to give informed consent. Exclusion criteria comprised: known allergies/sensitivity to any ingredient; prescription medicine use in the 7 days before test product use (excluding hormonal contraceptives and hormone replacement therapy); pregnant/trying to get pregnant; breastfeeding; currently using other ointments, gels or liniments; wounded/damaged/irritated skin in the application area; known skin sensitivity; diabetes and/or peripheral neuropathy due to other significant medical conditions; a need to apply heating pads/any form of device/compression bandages to the application area; use of OTC product within 24 hours of study product use; felt unwell/ill in previous 7 days; recent surgery or discharge from hospital stay; undergoing or scheduled for medical investigation for any medical condition or unexplained symptoms; or experience body pain on the day of the test; inability to follow study procedures; visual/smell impairment preventing sample assessment. The test intervention was a commercially available gel (Biofreeze® Gel, UK), a topical, cryotherapy pain relief formulation.
Subjects were required to participate in two phases of the study. Phase 1 was an objective evaluation of the impact of the test pain relief gel on skin surface temperature. All subjects were acclimatised to a consistent baseline temperature in a 22°C room for 10 minutes. A baseline skin surface temperature reading using a pre-calibrated temperature gun at a template-marked area of the subject’s dominant forearm (the test area, measuring approximately 6 inches x 2 inches) was recorded. Subjects applied a pre-weighed 0.5g of the pain relief gel (weighed to 0.01g accuracy) to the test area and placed their arm facing upwards on a marked area of a table where they were seated. As subjects were applying the product to a small, precise area during this phase, 0.5g was sufficient to provide coverage that mimicked usual consumer use. A skin surface temperature reading, using a RS PRO 8861 Infrared Thermometer, was taken by a single independent investigator at 6 inches (152.4 mm) from the test area at baseline and every 30 seconds post-application for 2 minutes, then at each minute for a further 9 minutes. Thermal imaging of the test and control areas (upper arm) was conducted throughout using a Topdon UK TC005 Model thermal camera, positioned perpendicular at 60cm to the test area and control area.
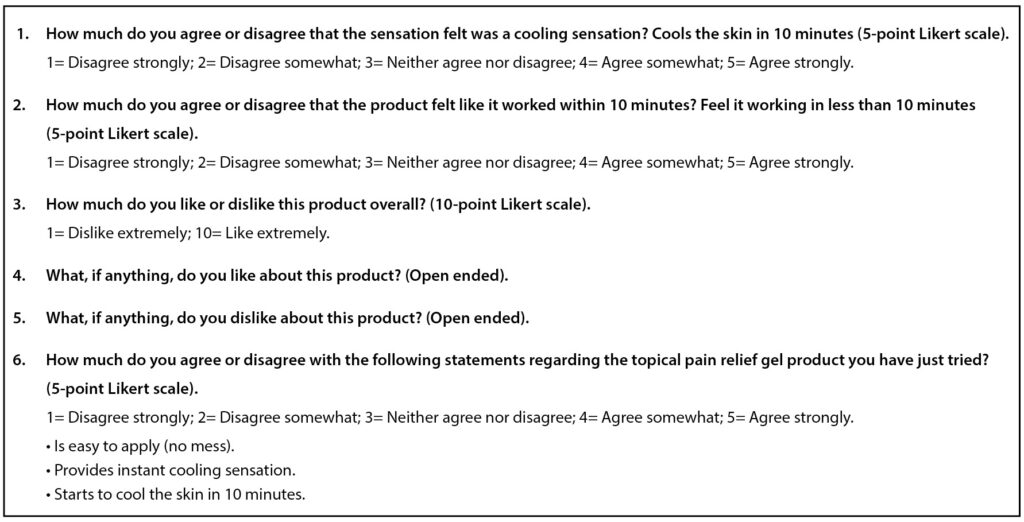
Phase 2 evaluated subjective skin cooling perception. This was conducted immediately post objective measurements after a wash-out period during which subjects washed their hands and forearm in cold water and then immediately applied 1g of the pain relief gel to their non-dominant forearm (i.e. opposite forearm to the test forearm in Phase 1 of the study) for 3 seconds. As subjects applied the product to their skin as they would with real-life use and were free to apply as they would normally, a larger quantity of product was provided in this subjective phase, versus the objective phase (1g versus 0.5g) to ensure reasonable skin coverage in line with real-life consumer use. Subjects were asked to record time to a perceived cooling sensation. They subsequently completed a questionnaire (see Table 1) on fast-acting cooling sensation, overall liking of product and agreement with product-related statements on 5-point and 10-point Likert scales. Subjects washed their hands and arm in cold water once the questionnaire was complete. The total study duration for each participant was 60 minutes. Statistical analysis considering both long-lasting and fast-acting data was via 2-tailed t tests performed at both 90% and 95% confidence to identify any significant differences between subgroups. The study was approved by the Reading Independent Ethics Committee.
Table 1: Post-study questionnaire
results
A total of 50 healthy subjects (25 males; 25 females) participated. The age split was as follows: 18–34 years: 13 (26%); 35–49 years: 17 (34%); and 50–65 years: 20 (40%). The statistical analysis utilised values at 95% significance.
Objective response: skin surface temperature reduction
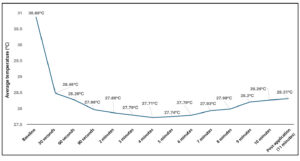
The average baseline skin surface temperature among subjects was 30.88°C. The pain relief gel reduced skin surface temperature from baseline temperature with reduction detected at the first recording at 30 seconds and at each time point interval (see Table 2). The peak average temperature drop of -3.172°C (10.27%) occurred at 4 minutes, p=0.05 (see Table 2 and Figure 1).
Table 2: Average skin surface temperature change of subjects from baseline at first to last timepoint (n=50)
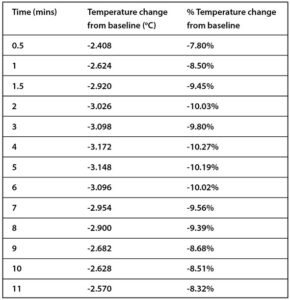
Figure 1: Average skin surface temperature change in subjects from pre- to post-application at each timepoint (n=50), p=0.05
When gender was considered, there was no significant difference in the skin surface temperature readings. When age was considered, there appeared to be a greater skin surface temperature reduction in those aged 50-65 years vs those aged 18–34 years, however this was only significant at 30 seconds and 2 minutes post-pain relief gel application, p=0.05. Between the 18–34 years and 35–49 years groups there was a significant difference at 30 seconds, p=0.04, but not at 2 minutes, p=0.06.
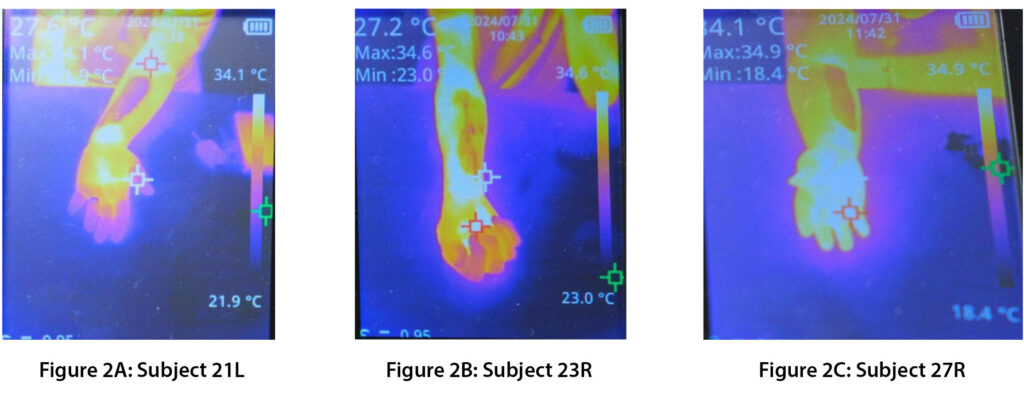
Objective response: thermal imaging skin surface temperature reduction
Thermal images recorded during the study showed a marked difference in the skin temperature of the test and control areas throughout the study period (see Figure 2).
Figure 2: Sample thermal images of skin temperature changes from test areas (dark areas on forearm indicate cooled skin)
Subjective response: perception of cooling sensation
All subjects (100%) reported a cooling sensation within 2 minutes of the pain relief gel application, 88% recorded a cooling sensation within 30 seconds and 96% in less than a minute. Subjects’ average time to record a cooling sensation was 14.84 seconds. All subjects (100%) agreed strongly or somewhat that the pain relief gel had a cooling sensation, with 94% agreeing strongly or somewhat that they perceived it had an ‘instant’ cooling sensation, in response to a question determining their level of agreement that the product provided an instant cooling sensation.
In terms of user acceptability, 82% of subjects agreed strongly or somewhat that the pain relief gel was easy to apply with no mess, 92% agreed that, overall, they liked the pain relief gel.
Considering subjects’ response to an open-ended question on positive product attributes, the pain relief gel’s cooling effect ranked highest (53%), after fast-acting (43%), fragrance (41%) and easy application (27%). In terms of negative product attributes, 45% of subjects reported there was nothing they disliked about the pain relief gel, while 16% stated fragrance, 12% difficulty in applying, 12% consistency, 8% sensation on skin and 6% the product’s colour.
Adverse events
Just 2 subjects (4%) reported adverse events after using the pain relief gel, both of which were fragrance-related. One reported the strong fragrance affected their throat, while the other noted mild stinging of the eyes. In both subjects symptoms resolved within 24 hours.
discussion
This study examined the skin cooling effect of an OTC topical cryotherapy pain relief gel (Biofreeze®). It demonstrated that the pain relief gel objectively reduced skin surface temperature, as shown by both temperature gun readings and thermal imaging recording. In addition, subjective perception demonstrated that more than 9 out of 10 subjects felt an ‘instant’ cooling sensation and had a positive liking for the product.
These results are unsurprising as a 1°C degree reduction in temperature results in a skin cooling sensation30,32 and, by the time of the first objective measurement at 30 seconds, the pain relief gel application resulted in an average -2.408°C skin temperature reduction in subjects. Subjective response found 88% of subjects felt a cooling sensation within 30 seconds. An earlier skin temperature reading at around 15 seconds could have provided objective validation for subjects’ perception that the average time to feel a cooling sensation was 14.84 seconds. This rapid temperature reduction and cooling sensation may be due to the fact that localised cooling can arise through the evaporation of cooling agents contained within the cryotherapy pain relief gel18. As alcohol has a low evaporative heat, it transiently decreases skin temperature to stimulate the TRPM8 cold receptors18.
As such, gels, such as Biofreeze®, could provide the benefits of convenient cryotherapy while avoiding the potential for ice-induced adverse events, such as pain, burns, numbness and frostbite18, as demonstrated by the low adverse event rate in this study with no cutaneous reactions. The damaging effects of ice are seen at lower temperatures (<15°C)30, which is considerably lower than the surface skin temperatures reached in this study. While cryotherapy is an accepted pain modality, data are lacking on the optimum level of cooling required to elicit analgesia. Research in 16 healthy subjects from 50 years ago suggests ice massage induced pain relief only after extreme localised cooling occurred, with skin temperatures reduced to, and maintained below, 13.6°C33. Not only does this temperature fall into the noxious region where adverse effects can occur30, achieving this low temperature can be difficult in reality as it necessitates the user to apply ice for 15-30 minutes before such a reduction can be reached34. Other data show interventions that result in modest cooling can elicit analgesia in animals via activation of the TRPM8 receptors25. Further work is required to compare the optimum skin temperature reduction for analgesia with traditional cryotherapy versus cooling gel cryotherapy.
What is not in doubt are results of meta-analyses and systematic reviews that have examined the efficacy of cryotherapy in MSCs. Ice massage improved range of movement, function and knee strength, while cold packs decreased swelling in people with OA35. Cooling, in particular cold water immersion, significantly affected the symptoms of delayed-onset muscle soreness36. There is moderate evidence to support cryotherapy post-surgically to reduce pain and improve range of motion, while a lower certainty of evidence supports its use as beneficial in acute pain and injury or chronic pain37. The use of cryotherapy post total knee replacement surgery found subjects had 2.9 times less pain than those not using cryotherapy38. Efficacy data in Biofreeze® has found benefits in a wide range of MSCs, such as neck pain, acute low back pain, knee pain due to OA, hand/arm pain due to carpal tunnel syndrome and muscle soreness39-43.
For healthcare professionals, including community pharmacists, having an effective and convenient to use OTC treatment option for the management of MSCs is important. Recent research among French community pharmacists found a high percentage agreed that some patients wanted natural or non-medicated treatments and they see an increasing number of patients requesting such treatments44.
Limitations of this study include: 1) the population was healthy and it is not known if the findings are equally applicable to those with MSCs; 2) the study did not compare against traditional cryotherapy in the form of ice application to determine comparable response; 3) the study was not blinded and subjects were non-rejectors of both cryotherapy gels and the brand, which may have biased the subjective results, although this had no impact on the objective measurements; 4) the skin temperature gun was hand-held by an independent investigator rather than being in a fixed position, which could have had a minor effect on positioning accuracy between subjects and in-subject readings. However, the same investigator undertook all tests to minimise inter-person variability. In addition, this would have had no bearing on the overall skin temperature readings.
conclusion
This study demonstrates that in healthy adults, a topical cryotherapy pain relief gel (Biofreeze®) had a proven cooling effect across all subjects as shown by a reduction in skin surface temperature measurements and captured in thermal imaging. Subjects perceived this cooling effect as ‘instant’, with proven reduction in skin temperature within 30 seconds. This was further confirmed by a subjective response, with the average time to cooling within 15 seconds. This ‘instant’ cooling action may be due to the evaporative action of the gel’s alcohol content; further work is required to determine the speed of onset of the analgesic action of Biofreeze®.
Correspondence to: Franciele Alves, Reckitt Ltd, Turner House, 103–105 Bath Road, Slough, UK.
Email: franciele.alves@reckitt.com
Authors’ contributions: FA commissioned the sensorial study from Blue Yonder. All authors contributed to the study methodology and questionnaire and supervised the data collection and analysis undertaken by Blue Yonder. All authors were involved in the initial drafting and critically reviewing subsequent drafts. All authors read and approved the final version of the manuscript prior to submission.
Authors’ declarations of personal interests: All authors are employed by Reckitt Ltd.
Declaration of funding interests: This study was undertaken by Blue Yonder and funded by Reckitt Ltd. Hollie Bell and Chloe Million from Blue Yonder reviewed the initial draft for accuracy and statistical checking. Statisticians at Blue Yonder reviewed subsequent drafts and approved the paper for accuracy. Reckitt Ltd employees Dr Bill Laughey, Senior Medical Scientist, and Adrian Shephard, Global Medical Marketing Director, reviewed and contributed to revisions of the manuscript. Marianne Mac Donald of Health Ink Ltd provided editorial support in the preparation of this manuscript, under the direction of the authors and reviewers, funded by Reckitt Ltd.
References
- Gill TK, Mittinty MM, March LM, et al. Global, regional, and national burden of other musculoskeletal disorders, 1990-2020, and projections to 2050: a systematic analysis of the Global Burden of Disease Study 2021. Lancet Rheumatol. 2023;5(11):e670–e682.
- Musculoskeletal health. Factsheet. [Internet]. Geneva: World Health Organization; 2022 Jul 14. Accessed February 17th, 2025. Available at: https://www.who.int/news-room/fact-sheets/detail/musculoskeletal-conditions.
- Steinmetz JD, Culbreth GT, Haile LM, et al. Global, regional, and national burden of osteoarthritis, 1990–2020 and projections to 2050: a systematic analysis for the Global Burden of Disease Study 2021. Lancet Rheumatol. 2023;5(9):e508–e522.
- Black RJ, Cross M, Haile LM, et al. Global, regional, and national burden of rheumatoid arthritis, 1990–2020, and projections to 2050: a systematic analysis of the Global Burden of Disease Study 2021. Lancet Rheumatol. 2023;10(5):e594–e610.
- Verhaar, JAN, Kjærsgard-Andersen, P, Limb, D, Günther, K-P and Karachlios, Th (Eds). The EFORT White Book: “Orthopaedics and Traumatology in Europe”. [Internet]. Lowestoft (UK): Dennis Barber Ltd; 2021.
- Lewis R, Gómez Álvarez CB, Rayman M, Lanham-New S, Woolf A, Mobasheri A. Strategies for optimising musculoskeletal health in the 21st century. BMC Musculoskelet Disord. 2019;20:164.
- FIP. Managing musculoskeletal pain in the community pharmacy. Report from an international insight board. 2024. Accessed February 17th, 2025. Available at: https://www.fip.org/file/5758.
- Nagy G, Roodenrijs NMT, Welsing PMJ, et al. EULAR points to consider for the management of difficult-to-treat rheumatoid arthritis. Ann Rheum Dis. 2022;81(1):20-33.
- Moseng T, Vliet Vlieland,TPM, Battista S, et al. EULAR recommendations for the non-pharmacological core management of hip and knee osteoarthritis: 2023 update. Ann Rheum Dis. 2024;83(6):730–740.
- Martin RL, Davenport TE, Fraser, JJ, et al. Ankle stability and movement coordination impairments: Lateral ankle ligament sprains revision 2021. Clinical practice guidelines linked to the international classification of functioning, disability and health from the Academy of Orthopaedic Physical Therapy of the American Physical Therapy Association. J Orthop Sports Phys Ther. 2021;51(4):CPG1-CPG80.
- Osteoarthritis in over 16s: diagnosis and management. London: National Institute for Health and Care Excellence (NICE);2022 Oct 19. PMID: 36745715. Available at: https://www.nice.org.uk/guidance/ng226.
- Rheumatoid arthritis in adults: diagnosis and management. London: National Institute for Health and Care Excellence (NICE); 2018 Jul 11. PMID: 30102507. Accessed February 17th, 2025. Available at: https://www.nice.org.uk/guidance/ng100.
- Low back pain and sciatica in over 16s: assessment and management. London: National Institute for Health and Care Excellence (NICE); 2020 October 12. PMID: 33090750. Accessed February 17th, 2025. Available at: https://www.nice.org.uk/guidance/ng59.
- WHO guideline for non-surgical management of chronic primary low back pain in adults in primary and community care settings [Internet]. Geneva: World Health Organization; 2023. PMID: 38198579. Accessed February 17th, 2025. Available at: https://www.who.int/publications/i/item/9789240081789.
- Mangin D, Bahat G, Golomb BA, et al. International Group for Reducing Inappropriate Medication Use & Polypharmacy (IGRIMUP): Position Statement and 10 recommendations for action. Drugs Aging. 2018;35(7):575–587.
- Allan R, Malone J, Alexander J, et al. Cold for centuries: a brief history of cryotherapies to improve health, injury and post‑exercise recovery. Eur J Appl Physiol. 2022;122(5):1153–1162.
- Tipton MJ, Collier N, Massey H, Corbett J, Harper M. Cold water immersion: kill or cure? Exp Physiol. 2017;102(11):1335–1355.
- Page P, Alexander L. The clinical effectiveness of Biofreeze® topical analgesic on musculoskeletal pain: A systematic review. J Perform Health Res. 2017;1(1):1–10.
- Kwiecien SY, & McHugh MP. The cold truth: the role of cryotherapy in the treatment of injury and recovery from exercise. Eur J App Physiol. 2021. 121(8):2125–2142.
- Clinical Knowledge Summaries. Sprains and strains. Scenario: Management. London: National Institute of Health and Care Excellence (NICE). September 2020. Accessed February 17th, 2025. Available at: https://cks.nice.org.uk/topics/sprains-strains/management/management/.
- Kwiecien SY. Is it the end of the ice age? Int J Sports Phys Ther. 2023;18(3):547–550.
- Algafly AA, George KP. The effect of cryotherapy on nerve conduction velocity, pain threshold and pain tolerance. Br J Sports Med. 2007;41(6):365–369.
- Green BG, McAuliffe BL. Menthol desensitization of capsaicin irritation: Evidence of a short-term anti-nociceptive effect. Physiol Behav. 2000;68(5):631–639.
- Bini G, Cruccu G, Hagbarth K-E, Schady W, Torebjörk E. Analgesic effect of vibration and cooling on pain induced by intraneural electrical stimulation. Pain. 1984;18(3):239–248.
- Proudfoot CJ, Garry EM, Cottrell DF, et al. Analgesia mediated by the TRPM8 cold receptor in chronic neuropathic pain. Curr Biol. 2006;16(16):1591–1605.
- Garcia C, Karri J, Zacharias NA, Abd-Elsayed A. Use of cryotherapy for managing chronic pain: An evidence-based narrative. Pain Ther. 2021;10(1):81–100.
- Pertusa M, Solorza J, Madrid R. Molecular determinants of TRPM8 function: key clues for a cool modulation. Front Pharmacol. 2023;14:1213337.
- McKemy DD, Neuhausser WM, Julius, D. Identification of a cold receptor reveals a general role for TRP channels in thermosensation. Nature. 2002;416(6876):52–58.
- Peier AM, Moqrich A, Hergarden AC, et al. A TRP channel that senses cold stimuli and menthol. Cell. 2002;108(5):705–715.
- McKemy, DD. Molecular basis of peripheral innocuous cold sensitivity. Handb Clin Neurol. 2018;156:57–67.
- Stinson RJ, Morice AH, Sadofsky LR. Modulation of transient receptor potential (TRP) channels by plant derived substances used in over-the-counter cough and cold remedies. Respir Res. 2023;24(1):45.
- Erpelding N, Moayedi M, Davis KD. Cortical thickness correlates of pain and temperature sensitivity. Pain. 2012;153(8):1602–1609.
- Bugaj R. The cooling, analgesic, and rewarming effects of ice massage on localized skin. Physical Ther. 1975;55(1):11-19.
- Wang Z-R & Ni G-X. Is it time to put traditional cold therapy in rehabilitation of soft-tissue injuries out to pasture? World J Clin Cases. 2021;9(17):4116-4122.
- Brosseau L, Yonge KA, Robinson V, et al. Thermotherapy for treatment of osteoarthritis. Cochrane Database Syst Rev. 2003, Issue 4. Art. No.: CD004522.
- Hohenauer E, Taeymans J, Baeyens J-P, Clarys P, Clijsen R. The effect of post-exercise cryotherapy on recovery characteristics: A systematic review and meta-analysis. PLoS One. 2015;10(9): e0139028.
- Klintberg IH, Larsson ME. Shall we use cryotherapy in the treatment in surgical procedures, in acute pain or injury, or in long term pain or dysfunction? – A systematic review. J Bodyw Mov Ther. 2021;27:368–387.
- Yildiz T, Topcu O, Avcu C. The effect of cryotherapy on pain in patients with total knee replacement surgery: a meta-analysis. Acta Orthop Belg. 2024;90(1):123–129.
- Bishop BN, Jacks DE, Greenstein JS, Topp R, Huffman A. The short-term effects of 2 different cryotherapy methods on acute and subacute, noncomplicated, bilateral neck pain. J Perform Health Res. 2017;1(1):11–17.
- Zhang J, Enix D, Snyder B, Giggey K, Tepe R. Effects of Biofreeze and chiropractic adjustments on acute low back pain: a pilot study. J Chiropr Med. 2008;7(2):59–65.
- Topp R, Brosky JA Jr, Pieschel D. The effect of either topical menthol or a placebo on functioning and knee pain among patients with knee OA. J Geriatr Phys Ther. 2013;36(2):92–99.
- Sundstrup E, Jakobsen MD, Brandt M, et al. Acute effect of topical menthol on chronic pain in slaughterhouse workers with carpal tunnel syndrome: triple-blind, randomized placebo controlled trial. Rehabil Res Pract. 2014:2014: 310913.
- Johar P, Grover V, Topp R, Behm, DG. A comparison of topical menthol to ice on pain, evoked tetanic and voluntary force during delayed onset muscle soreness. Int J Sports Phys Ther. 2012;7(3):314–322.
- Alves F, Angier K, Shephard A. French community pharmacists’ attitudes towards a branded, non-medicated, over-the-counter cold therapy for the topical relief of pain, in comparison with NSAIDs. Poster PPR-011. Poster presented at the 82nd FIP World Congress of Pharmacy and Pharmaceutical Sciences, Cape Town, South Africa, 1–4 September 2024.
